Homelessness in America
John is a 28-year-old male. In his early 20s
he was in college and living with his girlfriend. At that time, he began going
through periods of extreme depression and was unable to get out of bed and then
would cycle to hyper manic states where he couldn’t focus in class and would
make inappropriate outbursts. He was on insurance through college and went to a
doctor who diagnosed him with bipolar disorder. He was put on medication at
that time. However, the college did not have a medication plan, so he quickly
ran out of money to afford the medicine and began the same cycle. Due to this
he quickly flunked out of school.
He got a job at a grocery store that did not
have insurance benefits, so he was unable to get any medicine. After 6 months
he lost that job, and his girlfriend broke up with him due to his increasingly
erratic mood. He found himself living in his car. He got a job at a gas station
and was allowed to keep his car there so he could work and live. He could only
afford minimal food due to his part-time wages and most of that was through his
discount at the gas station, so it was not very healthy. Due to this he started
to develop some concerning numbness in his fingers and would find himself
overly tired. One day the owner of the gas station found him passed out in his
car. He was taken to the hospital via ambulance where he was placed on life
support and his blood sugar was found to be in the 300s. He was put on insulin
and given his psychiatric medicine. Once he was “healthy”, he was discharged
back to his car and his work at the gas station.
Very soon his mood fluctuations became worse
and his work sluggish due to his inability to get insulin to control his blood
sugar. He lost his job and his car ended up being towed. Since he did not have
money to get his car out of the impound lot, he found himself sleeping on the
street and begging for any money he could get. About once a week he would go into
the hospital where he found that if he threatened suicide, he could get a bed
and a meal for a night while he was on suicide watch. His moods became
increasingly erratic, and he would find himself taken into police custody after
calls from various people calling his behavior suspicious.
His health continued to decline, and his
kidneys began to fail. He was put on dialysis and set up with a dialysis clinic
to see to his needs. Since he was homeless, he was often unable to find a way
to get to treatments. Soon the dialysis clinic discharged him because he
was “noncompliant”. He began to sporadically go into the Emergency room when
things would get so bad that he could not stand it anymore. Soon the doctors
and nurses in the emergency room knew him well. He figured out how to “work the
system” for free meals and beds. He would go into the hospital, be stabilized
and then back to the street.
At 28
years old John is homeless and using the emergency room to treat any health
needs. He has uncontrolled diabetes, uncontrolled bipolar disorder and is in
kidney failure. He has also lost the use of one of his hands and is in danger
of losing several toes. He sleeps on the streets because there are no shelters
he can stay in, and he can only eat when he is given a couple of dollars
begging or when he is in the hospital. With no address he cannot get insurance
so he cannot pay his hospital bills. Therefore, taxpayers are paying thousands
of dollars a month to keep him in health care through the emergency room.
This story is completely fictional but is based on many true stories of homeless individuals across the country. It is a true commentary on the state of health care and homelessness in America. Individuals and Families across the country are thrust into homelessness for millions of different reasons and their healthcare is precarious as best. It continues to cost taxpayers millions of dollars to keep this population healthy through the emergency room when it costs a lot less to find ways to house and find safe shelter for them to sleep.
Statistics
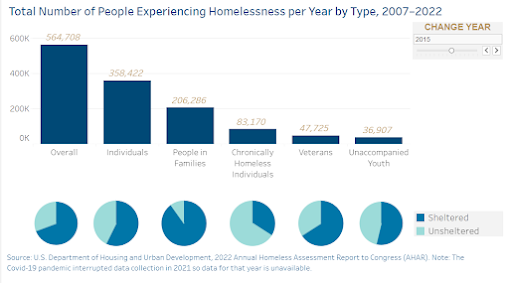
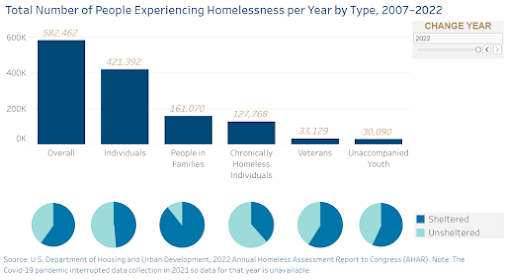
Graphics from State of Homelessness: 2023 Edition - endhomelessness.org
Public Health Implications
- Homeless individuals and families have higher
levels of health care need:
- Homeless individuals and families cost the
health care system:
- Permanent housing lowers health care costs:
o Health care costs are reduced by nearly 60% when a person finds a permanent place to sleep. (Green Doors, 2023)
Health IT/Data implications
- Public Health Departments need to have updated Health IT to have the ability to keep accurate health information for homeless individuals and families in the areas they serve. Between the public health department and the hospitals preventive services can be provided, but more consistent records are needed. (HealthIT.gov, 2023)
- An article in Digital Health by Alexia Polillo, Sophia Gran-Ruaz, John Sylvestre, and Nick Kerman, brings up the possibility of e-health services for homeless individuals and families so that they can be provided consistent medical care (Polillo et al., 2023). One issue with homelessness is that people are often moving from location to location without a consistent way to find preventive health services. E-health services might be a way to help these people find healthcare that is consistent. According to the authors more research is needed to determine the effectiveness of this option.
- Significant data is needed to determine the greatest areas of need and what is needed. More consistent records of homeless individuals from the time of first becoming homeless to follow-up after finding shelter is needed for conclusive research to be done. According to an article in the Lancet the longest follow up study was 6 years. A greater amount of data needs to be collected to do more consistent research. (Wickham, 2020).
Potential solutions
- Several hotels in Chicago were transformed into homeless shelters to great success during the past few years as concerns over COVID19 spread among the homeless population. (Johnson, 2021) In an effort to find temporary housing for individuals and families who are homeless, repurpose abandoned motels to make them into homeless temporary housing. In these living spaces, providing medical professionals who can provide preventive care and can provide mental healthcare services have helped improve the health of this population significantly. At the same time social workers can help those living there find jobs and permanent housing. (National Alliance to End Homelessness, 2023).
- A model for providing sleeping spaces for homeless individuals and families can be found in Springfield, MO. The model is called Eden Villages. These are small houses built for people who have been chronically homeless and/or have serious physical or mental handicaps that mean they have a greater need. The homes are built by volunteers and are communities where specific rules to be followed are required to live there. There is a small amount of rent that is required, and preventive medical services are available via donations from local churches and nonprofits (Eden Village, 2023).
- Another model in Sacramento County California are small sleeping buildings in an encampment where homeless individuals and families are given a clean and healthy place to stay for up to 90 days while they seek more permanent housing. There are clean communal areas and bathrooms with individual private sleeping areas. These people are chosen based on applications sent into a local nonprofit. They are given healthcare and other services to help them develop a better future. (Muegge, 2023)
Conclusions
Homelessness
is an epidemic in the United States that continues to get worse. Immediate
interventions are needed to change the lives of homeless individuals and
families. Still more interventions are needed to create change in the system
before the individuals and families become homeless. Data is needed to conduct
more research and create more interventions. Health IT can help to collect this
data and to keep track of health records to improve the healthcare of those who
are homeless. Collected data can help to pinpoint those who might be in need so
that interventions can be made before someone loses their place of living. The
combination of local governments, public health departments, and hospitals can intervene
to help this population and, in the process, help to bring preventive healthcare
to more people, save lives and ultimately save money for the taxpayers.
Eden
Village. (2023). Imagine a city where no one sleeps outside. Eden
Village: Tiny Home Communities for the Chronically Homeless.
https://edenvillageusa.org/
Green
Doors. (2023). The cost of homelessness facts. Homes Through Community
Partnership. https://greendoors.org/facts/cost.php
HealthIT.gov.
(2023, May 16). Public health. HealthIT.gov.
https://www.healthit.gov/topic/health-it-health-care-settings/public-health#:~:text=Through%20the%20use%20of%20advanced%20technical%20solutions%2C%20public,essential%20to%20improving%20community%20and%20population%20health%20outcomes
Johnson,
C. (2021, April 19). When homeless people lived in hotels, here’s what we
learned. Chicago Tribune. https://www.chicagotribune.com/coronavirus/ct-prem-covid-19-homeless-shelters-hotels-20210419-3ihrct3rdvg65epnod6c2s5eru-story.html
Muegge,
A. (2023, August 14). Sacramento County opens tiny homes for homeless. Here’s
what the temporary shelter offers. https://www.sacbee.com/news/local/homeless/article278237088.html
National Alliance to End Homelessness. (2023, May 23). State of Homelessness: 2023 edition. Homelessness Data. https://endhomelessness.org/homelessness-in-america/homelessness-statistics/state-of-homelessness/
National
Alliance to End Homelessness. (2023, May 23). Hotel to Housing Case Studies.
Homelessness Data. https://endhomelessness.org/homelessness-in-america/homelessness-statistics/state-of-homelessness/
Polillo, A., Gran-Ruaz, S., Sylvestre, J., & Kerman, N. (2021). The use of eHealth interventions among persons experiencing homelessness: A systematic review. Digital Health, 7, 2055207620987066.
Stafford, A., & Wood, L. (2017). Tackling Health Disparities for People Who Are Homeless? Start with Social Determinants. International Journal of Environmental Research and Public Health, 14(12). https://doi.org/10.3390/ijerph14121535
Wickham,
S. (2020). Effective interventions for homeless populations: the evidence
remains unclear. The Lancet
Public Health, 5(6), e304–e305.
Comments
Post a Comment